Q fever, once known as query fever, is the most commonly reported zoonotic disease in Australia. While it rarely causes clinical disease in animals, those working across the livestock value chain are at risk, including farmers, farm workers, abattoir workers and agents.
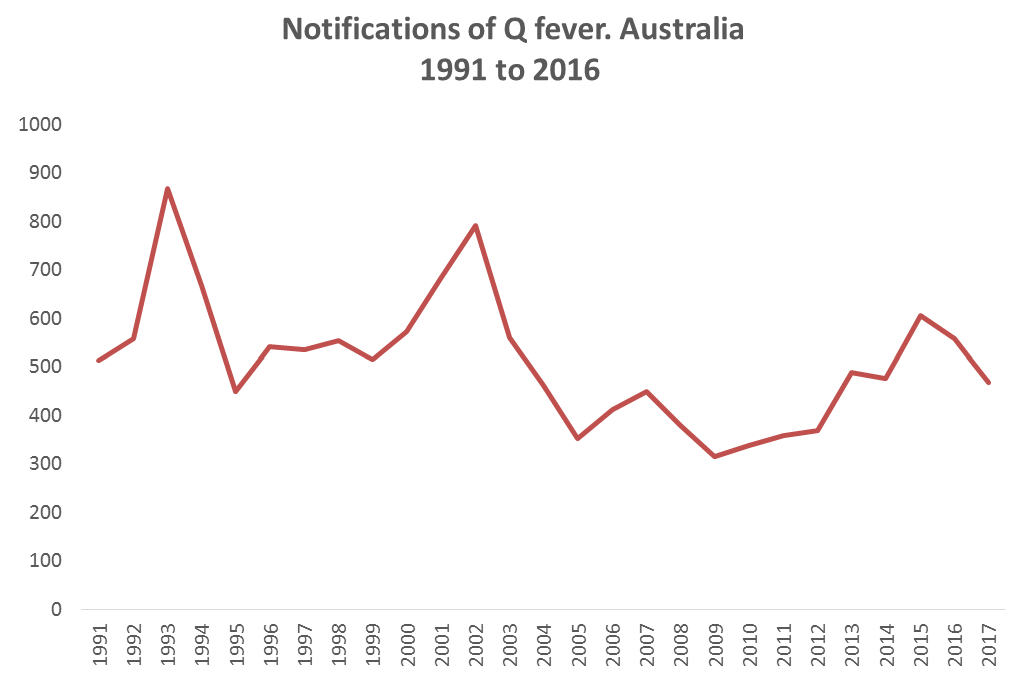
The most recent nationally subsidised vaccination program, implemented in 2002, reduced the number of reported Q fever cases in Australia. At the beginning of the campaign there were 792 cases reported annually in Australia. These numbers reduced to 352 when the campaign ended in 2005, as seen in Figure 1.
The vaccine has not been subsidised since and the number of reported Q fever cases has continued to rise.
An outbreak at a Victorian meat packing facility in 2016 resulted in a Q fever awareness campaign run by the Victorian Farmers Federation’s Livestock Group. The campaign promoted the dangers of Q fever and the importance of people getting vaccinated.
Why is it important?
Q fever costs the Australian livestock industry millions of dollars through lost employee productivity.
There is now an average of 520 cases reported each year over the last 5 years. All age groups are susceptible but the most commonly reported demographic is males between 45 and 69 years of age.
Symptoms of Q fever can be non-specific, including high fever, extreme fatigue, muscle and joint pain and severe headaches. Not surprisingly, the disease is often mistaken for the flu and goes untreated and so unreported.
Initial symptoms can evolve into acute Q fever and include symptoms such as hepatitis, pneumonia, headaches and, in rare cases, meningitis and encephalitis. The illness can be recurring, putting people off work for a minimum of two weeks with recovery potentially taking 12 months or longer.
In extreme cases, symptoms can develop further into chronic Q fever. This occurs in two forms, the most common form causing inflammation of the heart and heart valves, occurring in 60 – 70 per cent of those affected, and Post Q Fever Fatigue Syndrome, occurring in 10-20 per cent of those affected. Death occurs in less than five per cent of chronic Q fever cases and both forms are very difficult to treat and can have a significant impact the quality of life of those affected.
Who is at risk?
Q fever is caused by a bacteria Coxiella burnetti which can survive in air, soil, water and dust, and also on items such as wool, hides, clothing, straw and packing materials.
Individuals that come into contact with material contaminated by the bacteria are at potential risk of contracting Q fever. This includes:
- inhalation of droplets or dust
- contact with animal waste products including urine, milk, faeces or afterbirth
- contact with soiled straw or wool
- consuming un-pasteurised milk.
What can be done to reduce the impact?
Vaccination is more than 95 per cent effective in protecting against Q fever and is recommended for those working in the livestock industry. The process requires testing before vaccination to see if an individual has previously been exposed to Q fever, followed by a one-off vaccination that will protect against Q fever for life for those who haven’t been exposed.
To find a vaccinator in Australia visit www.qfever.org/findavaccinator.
As well as vaccination, basic hygiene practises may reduce the spread of Q fever. Such practices include:
- washing hands and arms in soapy water after handling animals or carcasses
- washing animal body fluids from work sites and equipment
- minimising dust and rodents in slaughter and animal housing areas
- keeping sheep and cattle yard facilities well away from domestic areas
- removing protective and/or other clothing that may carry infectious material before returning home
- properly disposing of animal tissues including afterbirth
- wearing P2 masks in high risk situations when unvaccinated.
Q fever is a debilitating, preventable disease which all livestock producers and workers are potentially at risk of contracting. Don’t put off getting vaccinated, get it done.
